Key Points:
- Core symptoms: Typically a sharp, alternating pain behind the buttocks (just above the pelvis to the left or right side) and stiffness to the lower back
- There is a simple blood test which can help expedite diagnosis
- If you experience any of the symptoms described below, contact your GP
Ankylosing spondylitis can be a lot of things.
At best it’s tiring, nagging and irritating…
At worst it’s so intensely painful and debilitating it can render you immobile.
But there is good news…
Many people have experienced real turnarounds with their ankylosing spondylitis.
They’ve gone from what can only be described as a painful and debilitating existence to one which is active and almost free of painful symptoms.
The purpose of this website is to help you find what works for you.
Before we get to some of the most common symptoms, let’s start with a disclaimer.
How ankylosing spondylitis will effect an individual patient will depend on a number of things, primarily:
1. Disease progression
2. Lifestyle factors
3. Individual biology
Like every disease it can effect different people in different ways.
However, there are number of common elements which the majority ankylosing spondylitis sufferers can relate to.
Typically the most frequently reported and painful symptoms are experienced in the lower back, specifically the sacroiliac (or SI) joints.
Symptom #1: Painful Flares
Location: Sacroiliac joint (inside the left or right buttock)
Feels like glass being pushed and twisted on a nerve
Duration: Typically flares can last around 2 weeks
Frequency: 10 – 12 times a year (can be a constant in more ‘active’ AS)
The sacroiliac joints are the area of the body that ankylosing spondylitis tends to hone in on.
These joints link your pelvis with your lower spine which is why any pain in this region feels like it’s coming from inside your buttocks.
In normal circumstances humans have no awareness or feeling in this part of the body.
In the same way we don’t notice our little toe unless we stub it or touch it.
However, ankylosing spondylitis patients experience a painful sensation in their sacroiliac joints when it becomes inflamed.
These attacks to the SI joints are known as ‘flares’.
- Typically it will effect one SI joint (or buttock) at a time
- The effects can last a few days (if you’re very lucky) or a few weeks.
Some patients with very active AS may experience this pain almost constantly unless they are treating it.
What does it feel like?
At it’s best it feels like an irritant. A niggling 1 or 2 out of 10 pain that you notice every time to take a step or you are positioned in a certain way.
When the pain is mild it has a kind of jagged, pinching, almost electric quality to it.
At its worst an SI joint flare is excruciating and can be completely immobilising.
Imagine someone pushing and twisting a shard of glass hard into a nerve at the base of your spine. It can feel like a near constant spasm.
At it’s most intense it can be a 10 out of 10 for pain. Screaming and all encompassing with extremely limited mobility.

Symptom #2: Concrete Like Stiffness
Location: From the base of the pelvis up to the mid spine
Feels like someone has poured concrete into your lower back and turned it into a solid block
Duration: 1 hour – 2 hours + (dissipates after activity)
Frequency: Daily for most
This is one of the most common and pervasive symptoms.
It’s also the one which is most often diagnosed as a lifestyle factor.
Because of this it can delay people getting tested for ankylosing spondylitis.
Typical explanations include: “it’s because you do desk work” or “you don’t exercise enough”.
As such patients are often send away with instructions to get up from their chair every 10 minutes and do more exercise.
Exercise is fantastically helpful for ankylosing spondylitis (the more movement the better). So in a way this is good advice but it can also result in delays to diagnosis.
Many patients go undiagnosed for years, decades even because they assume they just have chronic back pain.
Ankylosing spondylitis stiffness has a unique quality to it.
As the disease matures it can feel like someone has poured and set concrete down your spine.
It tends to run from about the middle of the back right down to the base of your pelvis.
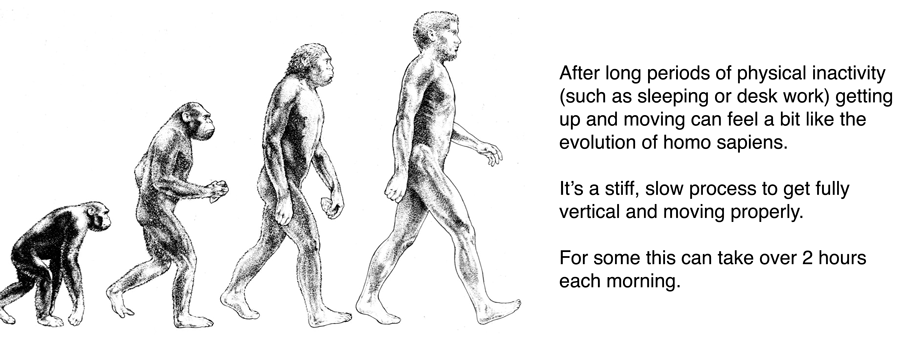
The famous ‘Evolution of Homo Sapiens’ drawing is a useful depiction of how it feels.
When you wake up each day it feels as if you are going from a hunched, rigid start and work your way up.
It requires a great deal of movement and getting going before you feel like you can walk more normally and without the ‘concrete effect’ in your back.
Symptom #3: Constant Exhaustion
Feels like you are tired all the time and could take multiple naps. There is a general feeling like you are constantly battling something
Duration: All day
Frequency: Most prevalent when in flare
When your body is in flare your immune system is actively fighting something.
This can be exhausting.
Think about how you feel when you are fighting off a nasty infection or cold. It’s the exact same thing.
You feel tired all the time, which in turn can make you feel foggy headed, irritable and on edge.
This is a particularly nasty side-effect of ankylosing spondylitis because it makes it hard to function in the day to day.
Napping can become a necessity for those who are able, but this brings with its own problems.
Inactivity and ankylosing spondylitis can exacerbate stiffness and pain.
That’s why it’s really important to get a diagnosis so that you can start treating the disease.
Symptom #4: Clicking Joints
Location: Ankles, knees, wrists, neck
Feels like everything with a joint is clicking at times
Duration: All day
Frequency: Most prevalent when in flare
As ankylosing spondylitis progresses you may find your joints start to click more and more often.
Ankles, knees, wrists are typical.
To being with this can be painless and more of an annoyance than anything.
Most patients find it’s particularly prevalent in the ankles and knees either when walking or going up and down stairs.
Left untreated this can cause real, long term problems so make sure you don’t suffer in silence.
If you are experiencing constant clicking of the joint, and you haven’t been diagnosed with ankylosing spondylitis, make sure you get this checked out.
As the joints rub together they can deteriorate which can cause further complications.
Don’t worry, there are things you can do to help resolve this!
Symptom #5: Restlessness
Location: Whole body
Feels like you can never quite get comfortable. You may find yourself squirming and jiggling in an effort to get settled.
Duration: All day
Frequency: Most prevalent at night or when sitting down
This one is harder to describe because it is subtle and a little less tangible.
Ankylosing spondylitis can give you severe restlessness.
Some people experience this more than others and there are those chalk it up to being a form of anxiety or OCD.
However there is a high incidence of restlessness in ankylosing spondylitis patients.
If you frequently find that you can’t lie still in bed or if you squirm in chairs a lot, this could be a symptom.
It is a general (and as odd as it sounds, largely subconscious) feeling of discomfort.
You don’t want to move about so much (especially if you are trying to sleep!) but it happens involuntarily.
Symptom #6: Night Cramps
Location: Legs
Feels like you are waking up several times a night cramping with a dull ache in your legs. You may find yourself constantly turning over to help self soothe
Duration: Night
Frequency: Regularly
Night cramps are cruel because they rob you of sleep.
One if the things you really need with ankylosing spondylitis is decent sleep and constant cramps during the night can decimate your sleeping patterns.
This can also tie in with overall restlessness and fatigue during the day.
Turning over on your side can offer temporary relief but many people with AS find they are still woken multiple times over the course of a night.
The good news is there are some straightforward, safe and effective things you can do to address night cramps.
Symptom #7: Rib and Breathing Pain
Location: Ribs
Feels like a type of flare with an electric, pinched nerve quality only in your ribs. Breathing can become extremely painful
Duration: All day
Frequency: 5 – 10 times a year
Not everyone with ankylosing spondylitis experiences rib pain.
It tends to occur where your rib cage joins to your spine, although it can feel like it is radiating out.
At worst this pain can feel like an SI joint flare. Breathing can be incredibly painful as if you are pushing your lungs against a pinched nerve.
At the lower end of the scale it can just be an irritating kind of fizzing, slightly electric pain that isn’t debilitating but is very distracting.
Rib flares tend to be less frequent but like SI joint flares they can take some time to go away.
The neck and shoulders are other areas that can also be affected.
Symptom #8: Uncomfortable Aches
Location: Arms or legs
Feels like you have bad blood coursing through your veins. A dull, alien ache in your arms or legs
Duration: Can last all day
Frequency: Sporadically
This is a very unique feeling and not one I’ve heard described elsewhere, at least not quite in this way.
It is likely a form of cramps but has a less visceral quality.
It feels as if someone has given you a blood transfusion but that they put in a bad batch, something that jars.
The sensation is like a slow dull ache flowing through your veins. This is primarily in the arms or legs.
While it is not debilitating it can cause some irritation and discomfort.
Wrapping Up
Ankylosing spondylitis, without treatment, is a progressive disease and gets worse over time.
This process can be slow and take years, or even decades. This can make it hard for patients and loved ones to identify the problem.
Symptoms are often dismissed as common back pain or further developments in symptoms are put down to old age or lifestyle.
Bear in mind that ankylosing spondylitis often displays symptoms in patients as young as 18 so if you experience flare like symptoms or any combination of symptoms above please book an appointment with your doctor.
Remember it absolutely doesn’t have to be all of the symptoms mentioned, different patients can experience different symptoms.



This is so fascinating to read and learn. Thank you..
Thanks Kevin, so glad you found it helpful. Feel free to shoot over any questions
Crazy all the things you wrote about I have experienced ,sometimes Dr’s make you feel as if you’re lying to get meds. I missed a couple days of work initially which forced a Dr’s appt. Was given steroids and a muscle relaxer it did nothing.I hate taking pills my gut has seen more ibuprofen that food in the last 4 months.Thank you for writing about this. You said blood work can diagnose this may I ask what is the test? I was actually going to schedule a MRI my self and pay out of pocket to see what was up with my lowerback. We have to be our own advocate. I’m thinking bloodwork would be a better option.Thank you so much for writing about this .
Hi Tammy, you’re so welcome. re: blood test, yes of course! There are a couple worth taking. 1. There’s a blood test you can take to see whether you have the HLA-B27 gene variant (this gene variant seems to be present in 90%+ people who have AS. Although even if you test negative it doesn’t mean you don’t have it). 2. They can look at your ESR and CRP levels in a separate blood test. These are blood inflammatory markers and can give them a good indication if your body is ‘fighting’ something. You’ll often see raised levels in autoimmune disease patients. Both can be useful pieces of the puzzle. I hope this helps!
Thank you! I had just started looking into intermittent fasting. I had tried KETO six years ago and had felt the best I had ever felt since childhood. Need to adjust my diet, thanks for the reminder.
That’s great, Linda! Hope it goes brilliantly. Feel free to ask any questions