Published: 2021 – Ongoing
Authors: Universidade do Porto, Portuguese Institute of Rheumatology, Centro de Investigação Interdisciplinar Egas Moniz
In Summary:
- The first major clinical study of the effect of a Low Starch Diet on ankylosing spondylitis patients since Ebringer’s early studies at the Middlesex hospital in London
- The study will look to explore the effect of a low starch diet on reducing Klebsiella gut bacteria and the effect this has on the disease progression and symptoms
- This study is currently underway…
Technical details from the study
Abstract:
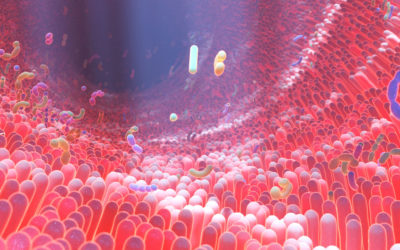
“The etiology of inflammatory bowel disease (IBD) remains elusive but it is believed to result from incompletely understood interactions between environmental triggers in a potentially genetically susceptible host and a subsequent aberrant immune response.
Its incidence is increasing worldwide at an unprecedented rate, outpacing what genetic influences alone could instigate. The increasingly integral role played by eating in social life has led patients to gravitate to diet and food in their consultations with physicians and other health care professionals, in an attempt to improve, control, or even “cure” IBD through diet.
Diet is a modifiable factor, and both patients and healthcare professionals have fuelled resurgent interest in the role of diet in maintaining IBD remission. Despite significant and increasing interest, there is a lack of credible evidence to support dietary modification or restrictions to prevent relapse of IBD.
However, recent studies have shown that more than half of the patients believe that diet plays an important role in triggering relapse, leading to self-imposed dietary restrictions, some of which can have adverse consequences.
This underpins the need for physicians and health care professionals to have a better understanding of dietary practices, in triggering, perpetuating, and improving IBD. This review examines and discusses the evidence behind this.”
Introduction:
“… The parallelism between “westernization” and particularly high dietary intakes of total fat (particularly animal fats, ω-6 polyunsaturated fatty acids (PUFA), milk fats), refined sugars, meat and lower intakes of fruit and vegetables, implicates diet in the great risk of developing IBD.
Diet may influence intestinal inflammation through several biologically plausible mechanisms including dietary antigen presentation, alterations in the gut microbiome, the mucosal immune system and epithelial barrier function among others…
… Dietary research is fraught with challenges, not in the least including the manifold variables in dietary intake, the proportion of food intake relative to other dietary components, the potential for complex interactions between food groups, variable food metabolism among individuals, and inherent differences in food products…”
Epidemiology:
“IBD prevalence is highest in northern America, northern Europe and Australia increasing globally, particularly in Asia with industrialization and westernization of lifestyles and diet.
Furthermore, immigration into areas of high incidence (e.g. South Asians migrating to northern America and the United Kingdom) also increases risk of IBD…
Several etiological theories link immigration and industrialization to IBD incidence and prevalence. The “hygiene hypothesis” suggests that reduced exposure to a variety of enteric organisms in early childhood from improved sanitization results in an ineffective and aberrant immune response.
Another theory, the “cold chain hypothesis,” argues that prolonged refrigeration of foods affects its bacterial content, promoting growth of psychotropic bacteria such as Listeria and Yersinia, both of which have been identified in patients with CD. Alterations in the intestinal microbiota increase susceptibility to aberrant immune responses triggering IBD.
A growing body of evidence suggests that dietary factors impact on microbiome composition and epithelial barrier function instigating and perpetuating IBD.”
Conclusions:
“The unprecedented global rise in incidence in IBD has clearly outpaced what genetic predisposition alone could instigate placing emphasis on environmental triggers in the etiology of the disease…
… the evidence for exclusive enteral nutrition in reducing symptoms and mucosal inflammation holds promise for the therapeutic benefit for certain diets and derived supplements.
These observations will serve to optimize clinical studies through identification of nocebo effects and pro-inflammatory food groups, enabling deeper mechanistic insights into the effects of food on the microbiota and the immune system.
It is plausible then, that in unraveling the mysteries of the microbiome, diet, and immune interactions, we may discover who “we are” through what we eat.”

0 Comments