Taha Rashid · Clyde Wilson · Alan Ebringer
Published: 11th November 2014
Abstract:
“Ankylosing spondylitis (AS) is a chronic inflammatory arthritis mainly affecting the spinal joints.
It would appear that the most likely causative agent in the development of AS is an environmental factor in the genetically susceptible, HLA-B27 positive, individuals.
Extensive data from several countries support the notion that Klebsiella pneumonia bacteria are the most likely culprit in the causation of AS.
These microbes possess antigens which resemble HLA-B27 and spinal collagens. Increased intake of high-starch diet is directly proportional to the gut associated bacterial load, especially in the large intestine, and among these microbial agents, Klebsiella is considered as one of the main constituting components.
Therefore, a low-starch diet intake alongside the currently used medical therapeutic modalities could be beneficial in the management of patients with early AS.
It is suggested that a change in the dietary habits from high protein, low-starch marine components to the Westernized high-starch diet among the Inuit peoples of Alaska and Canada could be considered as one of the main contributing factors in the increased prevalence of AS during the last few decades within this genetically unmixed native population.”
The role of Klebsiella in AS:
“… many reports support the role of Klebsiella microbes in the initiation and development of AS…
Cross-reactivity or the molecular mimicry hypothesis appears to be the main mechanism explaining the link between Klebsiella infections and the development of AS, on the basis that microbe-disease associated conditions such as rheumatic fever [34] is caused by the same mechanism.”
Starch, gut microflora and Klebsiella:
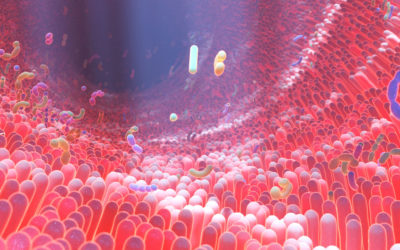
“There is a strong association between the axial spondyloarthritis including AS and gut inflammations.
There is also evidence for elevated levels of IgA, particularly secretory IgA antibody against Klebsiella antigens or Klebsiella cross-reactive antigens in active patients with AS.
These results support the notion that there is an association between AS and the mucosal immune responses in the form of elevated Klebsiella IgA antibodies.
The effect of low-starch diet intake on the level of total serum IgA was investigated. The mean concentration of the total IgA in 21 healthy volunteers ending 8-week low starch diet intake was dropped significantly when compared to the baseline values.
In another group of 11 healthy controls taking low-starch diet for 5 weeks, the mean serum secretory IgA level was shown to have decreased significantly by the end of the diet trial when compared to the start of study.
In a longitudinal open study carried out at the “London AS Clinic” a group of 36 patients with active AS had shown reductions in their ESR and total IgA, as well as a drop in their intake for the anti-inflammatory medicines after a 9-month follow-up following a decrease in their dietary intake of starch.

0 Comments