Published: January, 2015. Authors: Selma P. Wiertsema, Jeroen van Bergenhenegouwen, Johan Garssen and Leon M. J. Knippels
In Summary
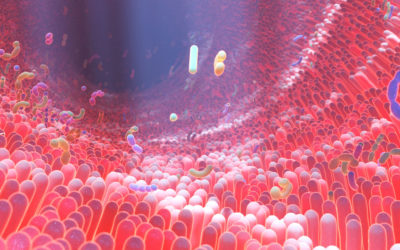
- 70% – 80% of your immune cells live in your gut
- The microbiota (bacteria, viruses, fungi, and protozoa) in your gut has to compete with different pathogens and also helps regulate your gut
- Your gut lining forms a barrier against pathogens (a damaged gut lining increases your risk of infection)
- Some of the substances your gut microbiota produces strengthen your body’s protective barriers and help your defence cells work better
Key Takeaways
Note: The following is my summary and take on this paper. Check out the full study here.
Most of your immune cells (between 70 – 80%) are located in the gut.
As a result there is a crucial interaction between:
1) Your gut microbiota (the non-human cells living in your gut)
2) Your gut lining
3) Your immune system
Your gut microbiota has to compete with different pathogens while also helping regulate your immune responses.
A healthy composition of microbiota supports your immune function, while ‘dysbiosis’ (when you have an imbalance of microbiota populations) can increase your risk of infection.
Your gut lining (or gut epithelium) forms a barrier against pathogens.
A mucus layer traps microbes away from epithelial cells and contains certain antimicrobial peptides. Microbes and their metabolites influence mucus production.
If you have an impaired barrier function it increases how susceptible you are to infection.
Now we’re going to get a little technical for a moment…
Your innate immune system recognises microbes via pattern recognition receptors (PRRs) like toll-like receptors (TLRs). PRR activation induces inflammatory cytokines and antimicrobial peptides.
Microbes shape PRR responses to maintain homeostasis (stability) and microbial metabolites like short-chain fatty acids support your barrier integrity and immune cell function.
In layman’s terms, your body has a natural defence system that spots what it sees as harmful microbes using special sensors, such as toll-like receptors. These can trigger a reaction that includes releasing molecules that cause inflammation and proteins to fight them off.
The microbes themselves can influence how these sensors respond to keep that balance (or homeostasis) in the body.
Some of the substances they produce can help strengthen our body’s protective barriers and help our defence cells work better.
Your gut microbiota also affects systemic immunity.
The microbiota in your gut influence your overall immune system.
Substances from these microbiota can travel in your blood and even boost immune cells far from the gut.
The gut bacteria also help certain immune cells work better. Some of these cells control inflammation, while others remember and fight off infections.
As an infant your gut microbiota guides your immune system development.
Reduced diversity has been linked to the development of allergies and in the elderly, immunosenescence impairs immune responses.
An inflamed microbiota with reduced diversity is common in older people and likely increases infection susceptibility.
Clinicians are now starting to consider the microbiota-immune interactions in infectious disease management.
Antibiotics are now a hot topic.
Antibiotics disrupt the microbiota, increasing pathogens like Clostridium difficile (sometimes known as C-diff, a really nasty infection that can lead to life-threatening inflammation of the colon).
Probiotics may reduce diarrhea and respiratory infections, but so far the evidence is mixed. The composition of your microbiota may also impact vaccine responses.
Diet has a powerful influence on your microbiota and immunity.
Fibers and prebiotics promote beneficial bacteria and metabolites that boost immunity and probiotics compete against pathogens.
Synbiotics combine pre- and probiotics.
A randomised trial found a synbiotic reduced sepsis in infants.
We’re increasingly finding that personalised nutrition based on genetics, phenotypes and habits may well optimise the immune response.
In summary, intricate gut microbiota-immune interactions affect local defences and systemic immunity throughout your life.
Optimising these interactions via diet can help improve infectious disease prevention and outcomes. However, more research is still needed.
Key Quotes from the Paper
Abstract
“Infectious diseases and infections remain a leading cause of death in low-income countries and a major risk to vulnerable groups, such as infants and the elderly.
The immune system plays a crucial role in the susceptibility, persistence, and clearance of these infections. With 70–80% of immune cells being present in the gut, there is an intricate interplay between the intestinal microbiota, the intestinal epithelial layer, and the local mucosal immune system.
In addition to the local mucosal immune responses in the gut, it is increasingly recognized that the gut microbiome also affects systemic immunity.
Clinicians are more and more using the increased knowledge about these complex interactions between the immune system, the gut microbiome, and human pathogens.
The now well-recognized impact of nutrition on the composition of the gut microbiota and the immune system elucidates the role nutrition can play in improving health.
This review describes the mechanisms involved in maintaining the intricate balance between the microbiota, gut health, the local immune response, and systemic immunity, linking this to infectious diseases throughout life, and highlights the impact of nutrition in infectious disease prevention and treatment.”
Protection from Infections in the Gastro-Intestinal Tract: The Gut Microbiota and Epithelial Barrier
“There are three main hurdles that pathogens need to overcome to cause an infection in the gastro-intestinal (GI) tract: the intestinal microbiota, the intestinal epithelial layer, and the mucosal immune system.
The gut microbiota consists of a multispecies microbial community, consisting of bacteria, fungi, and viruses, living within a particular niche in synergy with the host [5]. Gut microbes and mammals have coevolved, so while microbes get a habitat to florish, the microbes regulate various host physiological functions, including regulating protective immunity against pathogens.
The composition of the gut microbiota is influenced by many factors, such as genetics; gender; age; socio-economic factors; nutrition; stress; and environmental factors, such as pollutants, antibiotics, and others—the so-called exposome.
Factors that disturb the microbial community structure and function, like the use of antibiotics, give space to opportunistic pathogens to colonize, grow, and persist. There are several mechanisms in which the microbiota ensures the prevention of colonization, overgrowth, pathogen-induced damage, and subsequent infection of the host. One mechanism is referred to as colonization resistance, where the commensal microbiota and invading microorganisms compete for resource availability, or niche opportunity, either in terms of nutritional or functional space.
To allow for this competition, bacterial cells continuously sense the environment using signaling molecules accumulated during bacterial replication, in that way monitoring population density and adjusting their gene expression accordingly, a mechanism called quorum sensing. The chemical signals lead to phenotypic changes of the bacteria that are associated with adherence, motility, and intestinal density, or with the excretion of protective compounds. The quorum sensing mechanism is used by commensals to ensure gut homeostasis, but is also used by pathogens to minimize host immune responses and increase pathogenicity.
Alterations to microbiota community structure, or a non-beneficial microbiota composition, potentially induced by diet, stress, and antibiotic and drug treatment, change the overall dynamics between the microbiota and host to result in low-grade inflammation, reduced colonization resistance, and altered infection susceptibility.
Next to the gut microbiota, the gut epithelial barrier plays a crucial role in protecting the host from infections by pathogens. This physical barrier that separates the commensal bacteria in the gut from the underlying tissues is a monolayer of cells joined through tight-junction-protein complexes.
The assembly of tight-junction complexes is a dynamic process, which can be disrupted by certain bacteria through the release of toxins. In addition, the epithelial cell layer is reinforced by a layer of mucus. This mucus lining of the epithelial barrier is among the first defense mechanisms of the intestinal epithelia against bacterial invasion, by preventing luminal and mucosal microbes from directly interacting with epithelial cells.
In addition to its function as a biophysical barrier, mucus also acts as a reservoir for host-produced antimicrobial molecules such as secretory IgA and defensins. Mucus production and degradation are governed via an intricate interaction between host and microbes regulated through host recognition of microbe-associated molecular patterns (MAMPs) and bacterial metabolites, and are thus susceptible to changes in the composition of the indigenous microbiota. Between mucus and microbes exists a reciprocal relationship where both changes in the host inflammatory state and changes in the microbiota composition can contribute to alterations in mucus production and composition, leading to increased susceptibility to infection.
The continuous interaction between the gut microbiota and intestinal epithelium leads to constant immune signaling. Regulation of this immune response, together with epithelial barrier integrity and permeability in the presence of commensal bacteria and invading pathogens, is essential for the maintenance of intestinal homeostasis. If this process is impaired, it can result in inflammation and infection”
Protection from Infections: The Effect of the Gut Microbiota on Systemic Immunity
“It is increasingly recognized that the gut microbiome, besides regulating the local mucosal immune system, also affects innate and adaptive cell-mediated systemic immune responses through a variety of mechanisms.
One mechanism involves the release of microbial soluble products, which translocate into the circulation and influence the activation of immune cells in the periphery.
Indeed, resident immune cells in organs distal to the gut can directly sense circulating microbial derived factors, and the absence of microbiota-derived signaling molecules causes alterations in immune function that lead to susceptibility to systemic infection…”
“The ability of signaling molecules released by the microbiota to enter the circulation also allows resident bacteria in the gut to already modulate the immune system during immune cell development during hematopoiesis and, in that way, influence the response to infection…”
“it is clear that a dysbiosis in the gut microbiota can lead to a reduced ability to induce a suitable local and systemic immune response, resulting in local inflammatory diseases, but also in diseases at distal sites. One distal site of specific interest is the airways and this specific, direct relationship between these two sites is being referred to as the gut–lung axis…”
“The microbiota and the immune system are closely related. Therefore, the increased infection rates observed in infants can also be correlated with changes in the microbiome. An infant may initially be exposed to bacteria in the womb and, after birth, intestinal colonization appears rapidly.
The colonization pattern is influenced by, among others, the mode of birth, genetics, whether the infant is being breastfed, geography, and the use of antibiotics. It has been proposed that the first 24 months of life represent a crucial developmental window for the establishment of the microbiome and may even determine the composition of the intestinal microbiota throughout life…”
The Effect of Nutrition on the Gut Microbiome, the Immune System and Infectious Diseases
“It is well-understood that nutrition has a large impact on the composition of the gut microbiota and the immune system and can, therefore, play a major role in the development of health and disease.
For example, the Western diet has been linked to enhanced inflammatory responses, by inducing epigenetic and transcriptional reprogramming of myeloid progenitors, thereby directly influencing the development of several non-communicable disease”
Conclusions
“As we are learning more about the intricate mechanisms by which the gut microbiota can influence local, innate, and systemic immunity, scientists and clinicians start using this information to develop approaches that target these processes, supporting the ultimate goal of improving prevention and treatment strategies for infectious diseases.
Such interventional strategies should take into account the significant variation in both the microbiome and immune responses between individuals, and will thus require a personalized approach. The fact that dietary interventions are able to induce a rapid change in microbiome function and downstream immune responses could be used to develop tailormade nutritional concepts that could influence the development and treatment success of infectious diseases.”

0 Comments