Today we’re going to look at your immune system, gut and the amazing world within your body known as the microbiome.
(There is more than one microbiome, and we’ll go into that in a moment!)
We’ll explore their different roles, the interplay between each and how they can affect your health.
It’s only really been in the last 20 years that we’ve become more aware of how significant a role the gut and the microbiome play in our overall health.
That’s why it’s so important to be careful about what we put in our bodies.
Let’s start with a crazy stat:
Over 50% of the cells in your body are alien. They’re non-human cells.
(Until relatively recently, microbiologists thought it could even be as high as 90%+!)
So what does this mean? Are we really part alien?
The short answer is yes!
You have human cells and trillions of ‘non-human’ microbiota which live inside your body and on your body.
They exist everywhere where there is life.
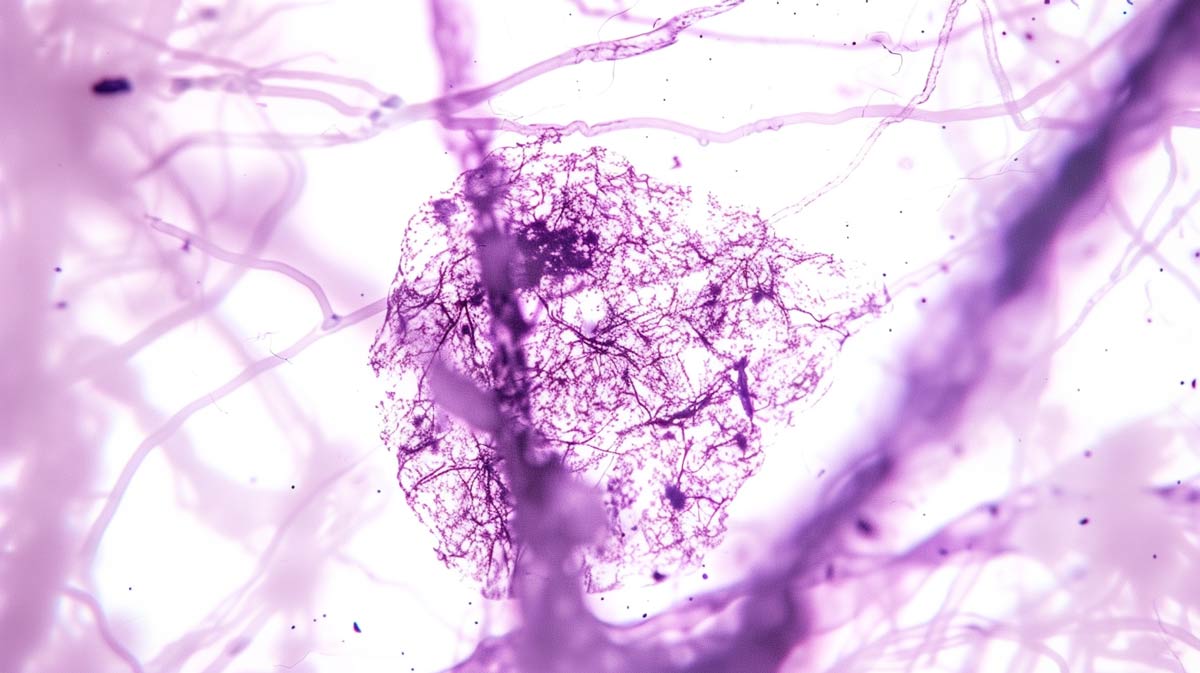
They consist of lots of tiny microorganisms – bacteria, viruses, fungi, archaea and eukaryotes and are known collectively as microbiota.
They’ve evolved with us since our existence on the planet.
(In fact, they’ve been here a lot longer).
For some of these species, we live together symbiotically. They help us and we help them.
But for the most part, they just exist. Sometimes they help us, sometimes they hinder us. They are just another organism trying to survive.
Obviously, there are more ‘negative’ ones (for us at least) and these can cause series infections and sickness.
But others help us process foods and the things we encounter in the environment and convert them into energy.
They’re essential.
We could not survive without them.
If you didn’t have a microbiome, particularly a gut microbiome, you would die. You would not be able to exist out in the world.
There is often a feeling with anything that’s bacteria or microbial that it must be some sort of germ that needs to be got rid of.
Actually, a lot of this stuff is absolutely essential to life.
That’s why when we’re looking to stay healthy, fit, full of energy and stave off illnesses and feel great, it’s essential to think about our microbiome.
We need to figure out how to maintain the best balance. To have less of the things that cause us problems and more of the things that help us.
50% of your body is made up of these microbiota

It can be hard to fathom.
This 50% figure is not in terms of size or weight.
It’s an estimate based on the total number of cells in your body.
You have tens of trillions of microbiota, and all of them are made up cells. You have human cells as well, and cells that make up things like bones are much larger and heavier.
So when we talk about the composition of a human, we’re literally talking about the number of cells.
Just because they may be physically smaller on an individual basis, that doesn’t mean that they should be underestimated…
Just like human cells they all have unique genetic makeups, and they can have really outsized effects.
They are extremely powerful in conjunction with our health.
Where do they live?
There are several microbiomes within the body.
You have, for example, the ocular microbiome (the world of microbiota that lives in your eye and interacts in your eye).
You’ve got a skin microbiome (the microbiota that live in your skin – that could be fungi, bacteria, all sorts of things. Some of them help us, some irritate us, and so on).
They are all around the body, you have lots of different microbiomes.
However, the gut microbiome is where somewhere between 90 and 95% of the microbiota in your body lives.
In other words, the bit that makes you ‘you’, or constitutes half of you as a human, lives inside your gut.
There’s an obvious reason for that.
So much of what they can thrive off and feed off comes in through food, water and everything else that comes directly into the gut.
That’s what makes it a great habitat for the vast majority of these microbiota.
70% of your immune system lives in your gut

The next piece of the puzzle is that 70% of your immune system lives in your gut.
Once you understand the role the microbiome plays, and how closely connected it is to the immune system, so many of modern health complaints start to make sense.
If you’re experiencing poor health or chronic pain – anything where their body is out of sync and not feeling as it should – the interplay between you gut microbiome and your immune system could be the root cause.
The immune system defends us against pathogens. It defends us against harmful bacteria, sickness, all of that kind of stuff and it acts as that defence unit inside our gut.
It operates elsewhere too, but 70% is in our gut because it is having to manage those enormous and diverse microbiota populations.
A big part of what your immune system does is help regulate and control that overall population of microbiota and ensure it doesn’t get out of whack.
For us to survive and thrive and do what we have evolved to do, there needs to be a balance in the populations.
If you’ve got too much of one strain of negative bacteria or fungi, you’re going to have problems.
So the big role of the immune system is to police that population in the gut.
(Hopefully, this is starting to give you an idea of how important what we put in our body is).
The vast majority of the microbiota in your body lives in your gut and the vast majority of your immune system is operating inside your gut.
This means that if there are:
a) Problems with the gut and gut lining
b) Problems with the microbial population living in the gut
You will to have all sorts of problems.
Ignoring the gut and microbiome can have a snowball effect of negative outcomes
Typically in medicine, in years gone past and still to an extent today, we treat the symptoms.
Someone is experiencing pain or having trouble sleeping so we develop and prescribe a pill, or an injection. This treatment will stimulate the body in the short term and offer a fast solution that feels like something’s working.
Indeed often it does work for a time – and in some cases can be essential, even life saving – but more often than not, it’s not tackling the root cause.
For many people, their issues stem from issues around their gut health.
Specifically what’s going into the gut and what’s happening with their immune system.
That brings us to a vital piece of this puzzle: the gut lining.
By gut lining, I mean the protective barrier that exists between your gut and the contents of your gut and the rest of your body.
It’s also known as the intestinal epithelium and forms the lining of both the small and large intestine. We’ll use the term ‘gut lining’ in this article for ease.
This gut lining or barrier is thin and vulnerable. In some places, it’s only one cell thick. If there’s a breach in the gut barrier, there can be real problems…
The lining has tight junctions and these regulate what passes through into the bloodstream and what doesn’t.
You want positive nutrients to pass through because that’s essential for us to survive and live and thrive and you want to keep the harmful stuff out.
The problem is when you have issues when either…
a) The gut lining is too easy to breach
b) The immune system is overworked, overwhelmed, or confused
c) A combination of the two
When this happens you can get all sorts of problems and disruption.
Intestinal permeability or ‘leaky gut’ could be the missing link behind hundreds of chronic health conditions

All of this leads us to something called intestinal permeability, sometimes known as ‘leaky gut’.
We now believe there is a strong correlation between leaky gut, autoimmune disease and a numerous other chronic health complaints.
Because this is a relatively new field of research often this goes often undiagnosed.
When was the last time your doctor or GP talked to you about leaky gut or the microbiome?
Leaky gut is where the gut lining becomes damaged and allows bacteria, toxins and even undigested food particles to leak into the bloodstream.
This can cause inflammation and changes to the gut composition known as dysbiosis.
Dysbiosis simply means an imbalance in your gut microbiota – that population of microbiota, bacteria, fungi and all the other microorganisms in your gut (some of which can be helpful and some not).
You’ve got too much of one, too little of the other, more of the bad, less of the good.
When this happens, it can cause inflammation and damage the gut lining which in turn leads to leaky gut.
This can wreak havoc.
When these substances ‘leak’ or get through, we see things like chronic inflammatory conditions.
And it has been linked (and is increasingly being linked) to a host of health conditions that have exploded in the modern age.
These include autoimmune diseases such as Crohn’s disease, rheumatoid arthritis, ankylosing spondylitis, celiac disease and more.
I’ve just mentioned a handful here, but there are dozens of different disorders.
There is strong evidence to suggest irritable bowel syndrome (IBS or IBD) is connected to leaky gut as well.
Increasingly, we’re finding it’s not just these diseases we’re familiar with, but also areas as seemingly unrelated as neurodivergence and cognitive decline (such as autism and Alzheimer’s) as well as mental health issues.
That’s why diet is such an important factor.
What you put in your body massively influences the composition of your gut.
The different populations of microbiota change according to what you eat.
For example, if you only consumed one type of food this would massively benefit and nourish certain microbiota over others and cause their populations to explode. Then you get an imbalance.
If these foods spark problems in your body, start damaging the gut lining and overworking the immune system, it can result in chronic pain and all sorts of health issues.
That’s why we need to look at what the big food producers are giving us, take stock of what we’re putting in our bodies and see what works best for us.
What’s ‘good’ and what’s ‘bad’ will be different for everyone

There are some general markers, though.
For most healthy people, foods that are high in fibre are generally beneficial. So too are prebiotics and probiotics (which is something we’ll cover in the future).
They support what we believe to be some of the most beneficial gut bacteria.
On the less healthy side, perhaps the easiest to identify and hopefully eliminate from your diet are ultra-processed foods.
This is (usually) anything that comes in a packet and has 5 or more ingredients.
Specifically it tends to be foods containing ingredients you don’t recognise or don’t see out in nature.
I quite like this phrasing (and I can’t take credit for this):
“Anything your grandmother wouldn’t recognise is probably ultra-processed food.”
Ultra processed foods tend to be ingredients developed in labs.
Some may well be inert (or not harmful) but we simply don’t know the long-term effects of all of the thousands of preservatives, additives, flavour enhancers, thickeners and more that now appear in our day to day foods.
Often these foods are high in sugar, trans fats and additives, as well as all of these unknowns.
These directly damage the gut, can mess with gut permeability and causes or exacerbate leaky gut.
If there’s one thing you take action on right now it would be this:
Cut ultra-processed foods from your diet.
The evidence is overwhelming how bad they are for us. In years to come I believe we’ll look as this as the ‘smoking’ health crisis of our time.
My experience with ultra-processed foods and chronic pain

I used to eat ultra-processed foods multiple times a day.
It was convenient, I loved the taste.
I also assumed that if the big supermarkets and food producers were advertising and selling them they couldn’t be that bad.
I now believe that this terrible diet accelerated and exacerbated my autoimmune disease progression.
While I wasn’t overweight when I was eating these foods, I felt awful.
I was exhausted and my joint inflammation was through the roof.
By my mid-thirties I was in pain all the time, and (what I now know to be) my ankylosing spondylitis symptoms were rapidly accelerating.
But at the time you don’t think to question the food you eat.
You blame “back problems”, “office work” or “getting older”.
I spent a small fortune on Pilates sessions (which are great), expensive desk chairs and pain gizmos.
While stretching exercises were also beneficial most of the interventions and gizmos did little more than make me slightly more comfortable while I was using them.
They never addressed the root cause: that my immune system was constantly fighting microbiota imbalances (dysbiosis) in the by now broken battleground of my gut.
I now manage my condition almost entirely through diet.
I do exercise regularly (and that’s important) but diet has been the most transformative element.
Getting rid of ultra-processed foods was top of the list.
Somewhat surprisingly, I don’t miss them at all anymore.
How to spot ultra-processed foods

If a product has a colourful label or several ingredients on the back, it’s probably ultra-processed.
That makes them really easy to spot.
Ultra-processed foods last longer and have been Frankenstein Monstered their way into explosive flavours and impossible textures and the food manufacturers want you to know all about them (at least the taste part) because:
a) They are cheaper to make
b) They have a much longer shelf life
c) They are addictive, so customers keep coming back for more
If a food producer’s primary goal is to make money (and this doesn’t apply to all producers) this combination is the goose that lays the golden eggs.
Creating addictive, repeat purchase products that last weeks, months or years on the shelves and cost very little to produce is their fast track to higher profits.
So it’s important to remember the incentive structures for the ultra-processed food manufacturers.
They’re interested in your money, not your health.
If you can try to cut down your intake (and ideally completely cut them out) you could experience a massive boost in health outcomes.
And finding alternatives is easy. In fact it’s easier because you’re less overwhelmed by choice.
Typically the real unprocessed or minimally processed foods in the supermarket are the domain of just a few aisles. The ones containing fresh fruit and veg and counters where they sell animal products.
NSAIDs like ibuprofen damage your gut lining
The next thing I wanted to mention was NSAIDs (non-steroidal anti-inflammatory drugs).
These are drugs like ibuprofen and other anti inflammatory drugs and painkillers.
They can be very effective – and important even – for short-term pain management.
If you are experiencing a lot of inflammation in a certain region, and nothing else is bringing the inflammation down, you could experience worse health outcomes so in these instances they can be an important part of your treatment.
However, repeatedly taking these drugs, over time, is damaging to the gut.
They cause massive irritation and inflammation to the gut lining.
The way I visualise it is that it’s a bit like throwing mini grenades at the gut lining.
You will tackle the inflammation in the short term, which is great, but what you’re doing long-term is eroding away that gut lining and opening yourself up to more problems in the future.
If you can find other, less invasive, ways of reducing inflammation (things like heat exposure, sauna, cold exposure, or changing the foods in your diet), that will be a massive boost.
You can tackle two things at once. You can start rebuilding your gut lining, calming your immune system, and readjusting the microbiota population in your gut so that you’ve got more of the good and less of the bad.
Alcohol, stress and antibiotics

We’ve looked at non-steroidal anti-inflammatory drugs and ultra-processed foods.
The next one, which I enjoy and am not very good at avoiding, is alcohol.
Alcohol, in large amounts, can cause inflammation and damage to the gut lining so it’s something to be aware of.
Some studies indicate that the odd (non binge) drink could be beneficial to your overall health, others say cut it out completely.
If you are someone who struggles with an inflammatory disorder (for example an autoimmune disease where excess inflammation is one of the symptoms) then the old adage less is more probably makes the most sense.
I know many people who have cut out alcohol completely as part of managing their pain symptoms who wish they had done it much sooner.
Remember, we are all different.
Our ancestors evolved in different environments with different levels of exposure and tolerance to alcohol. The impact a glass of wine or beer has on one person’s physiology could be completely different from someone half way across the world with a different genetic makeup and microbial composition.
See what works for you.
And bear in mind different drinks can have different impacts.
For example, in my case I seem to react more strongly to white wine and sparkling wines so I just cut them out of my diet for the most part. Instead I drink beer when socialising with friends and that – for me at least – has minimal impact.
As ever, if you zoom out and look at the bigger picture, a more nuanced approach makes sense in most cases.
Stress: the most under-talked about, under-targeted elements of health in the modern age
We only ever seem to talk about it in terms of mental health – we all know if you’re feeling chronically stressed, then it can make you feel miserable, anxious or depressed. However, what we don’t talk about is how stress itself, particularly chronic stress, physically impacts your health.
By chronic stress, I’m talking about worrying about things in the future that might never happen or worrying about things in the present that you can’t quite tackle or solve – maybe you’re doing a job where you feel a lack of meaning or you’ve got a boss who makes you feel anxious, and there’s this constant stream of stuff that you have to work through, and you’re worrying about bills you have to pay, all of this kind of stuff. This chronic stress that runs through your mind, the rumination, the anxiety, physically impacts your health. It directly impacts your gut lining and, as a result, affects the gut microbiome.
It’s essential to try and get on top of stress levels. I know that’s easier said than done because we can’t always pick the job we’re doing or what’s happening in our lives at a given moment.
One of the key things to identify with stress is that when we talk about stress, it’s not the immediate important stresses that come into our lives (maybe stress involved with something happening with your child or something you encounter in the day-to-day, or maybe you’re faced with quite a scary situation and you have to deal with it and tackle it, or maybe you’re encountering a physical stress).
Those kinds of stresses, where we have to problem-solve and deal with it, are healthy. The human body and the human brain have evolved to deal with that. It’s the chronic stress, typically when we’re dealing with more abstract ideas and issues that never quite go away and are constantly there like this horrible background erosion, that we need to address.
If you can do any work on that in terms of finding ways of giving yourself some space, whether that’s going for a walk in nature or talking to someone or spending more time around loved ones and putting the other stuff into perspective as best you can, that will help.
Stress alone can trigger an episode for people with adverse health conditions and autoimmune diseases. It’s that important. I and many people I know with autoimmune disease can do everything by the book in terms of diet and exercise, but then this big stress comes along, this feeling of lack of control and anxiety, and that can trigger a massive flare – physical debilitation. It’s horrendous. Do what you can to stay on top of your stress levels.
The next one many people will already know about is antibiotics.
Antibiotics are one of the most amazing modern miracles and incredible lifesavers, probably one of the biggest lifesavers we’ve ever come across. However, they are also natural-born killers. We put them into the gut, and they will hopefully help clear an infection or help us get rid of something we don’t want. But they also can often act a bit like napalm – you take an antibiotic, and while we try and specialise as much as we can, they are going to kill a lot of healthy stuff as well. They’re going to kill stuff we don’t want to lose in terms of population, and it’s this blanket bombing.
This is going to cause us some more of that gut dysbiosis. We’re going to get rid of stuff we want, and it’s also going to affect the gut lining.
In terms of antibiotics, obviously take them if you need them, but if it’s a case where you and your doctor feel something would probably pass if you didn’t take antibiotics and if you can let your immune system deal with it naturally, always try to take that option if it’s safe to do so.
High sugar diets are another big one – sugar is massively inflammatory and can promote the growth of bacteria and yeast and cause all sorts of problems in the gut. You’re going to find high sugar in ultra-processed foods and soft drinks by the gallon. Do what you can to avoid things that are high in sugar.
Things that are safe for sugar intake are fructose (sugar you can find in fruit). If you can, eat fruit naturally. Try to avoid blended fruit because that changes the food matrix, and what you’re going to get is a massive concentration of sugar in a way that your body can’t process. When you eat an apple, for example, your body and microbiome have evolved
When you actually eat an apple, for example, your body is evolved to, and your microbiome is evolved to, process that in the best way possible. That’s the way to go in terms of sugar intake.
Then, related to that, you have artificial sweeteners, which have become popular on the basis that too much sugar is bad for you and has become a sort of target market for the big food producers. However, the problem is they’re often producing these artificial sweeteners using ingredients that are even worse. Be really careful with these.
There are an increasing number of studies showing that these artificial sweeteners can negatively affect your gut microbiota and alter the gut’s microbial composition. In general, I would avoid artificial sweeteners. There are other ways to sweeten things – you can use honey (that’s going to be much better for you) or a type of monk fruit sweetener, which can be far less tough on the gut. There are different ways of getting that sweetness into the things you’re eating or drinks.
It’s not to say that all sugar is really bad. Refined sugar is not great, but in small quantities, it’s not going to kill you. However, the main things, like the popular soft drinks that we all know have several spoonfuls’ worth of refined sugar in them, are having this massive concentration going into your gut. It’s changing the composition of the microbes in your gut, damaging the gut lining and causing inflammation – a perfect storm of bad things.
When we try to remove that by introducing artificial sweeteners, which have effects that are even worse or as bad in some cases, it just causes more problems. When you’re looking for sweetness, think of things that occur in nature naturally – honey, molasses or fruit, all of those things that you might encounter in the real world.
Then we have food additives in general, which I touched on earlier. Those are things like the binders, fillers, emulsifiers, preservatives and artificial colourings. Again, you’re going to find those in ultra-processed foods.
We’re finding lots of evidence to show that this massively disturbs the gut microbiome, increases intestinal permeability and so on. The good news is that the last few I’ve talked about – sweeteners, high sugar, all of that kind of stuff – most of that is tied to ultra-processed foods. That’s where you’re going to find most of these problems.
If you’re eating foods as they come in the world, whether a mushroom, an apple, a floret of broccoli or any animal products that haven’t been processed or filled with rubbish, you’re going to get stuff which your body can cope with on the whole.
In many ways, there’s a lot of information to digest, but the solution is fairly straightforward: cut out the stuff that has these ‘Frankenfoods’ created in labs to taste better, be more addictive, have a longer shelf life and all of these things which are great for food producers and big businesses and shareholders but terrible for our health. Avoid that and focus on putting real things in your body that our microbiomes have evolved with over hundreds of thousands, millions of years.
The last one I wanted to talk about is ingredients that are going to be specifically problematic for you.
We’re not all the same. We all have different genetics and different compositions of microbiome and immune systems. A thing that might be beneficial to you or non-harmful to you might be absolute kryptonite for someone else.
The obvious example, which we’re all now aware of but weren’t just a few short decades ago, was coeliac disease and gluten. We know for these people, if they come into contact with gluten (maybe they eat pasta or bread containing gluten), they’re going to start to get horrible symptoms, really uncomfortable and quite debilitating in many ways, and fast-acting.
What we discovered was that the best and, in fact, the only way you can treat someone with coeliac disease is to say, don’t eat gluten, and when they don’t eat gluten, they don’t get any of these problems.
It’s a case of what you work well with individually with your specific composition. We will get there in terms of the science, in terms of people having DNA mapping and microbiome mapping and being able to pinpoint what the problems are. However, for many people, they won’t know.
This was the case for me – it took me 19 years to get my autoimmune condition diagnosis, my ankylosing spondylitis. I thought I had this mystery back pain, issues with something else, and the rashes and all of that stuff. I thought there was something completely unconnected, but it was all to do with this specific condition I have.
I found that for me and many others following the diet I’m following, removing starch and dairy works brilliantly well, as far as we can tell at the moment, as well as ultra-processed food, sugar and anything like that. Starch is going to be healthy for other people, so I wouldn’t recommend someone who thrives off that to start giving that up.
Similarly, the person with coeliac disease avoids gluten, but then you’ve got all these other conditions (SIBO, for example) and a whole set of different foods to look at. You’ve got FODMAPs and tons and tons of disorders connected with certain foods, triggering certain problems, creating gut dysbiosis, altering the populations of what that particular person’s genetic makeup and immune system can cope with, and what it can’t.
If you put the wrong population of microbiota in a person with a certain genetic makeup and immune system, there’s going to be havoc, and they’re going to feel tired, in pain, inflamed, physically debilitated and all of these things.
Often, it’s a case of sitting down, creating a spreadsheet and looking at what you’re eating, what makes you feel worse and what makes you feel better. If you can do that methodically, even just for a few months, you can get a good picture of what works for you.
That’s exactly what I did with my diet, and as I’ve said many times, it’s been life-changing. In another podcast, I will talk about how I went through this process myself, how I set up a food diary, and I will share the spreadsheet I made with you so that you can do it yourself.
You’ll be able to copy and paste and hopefully get on the road to figuring out what works best for you. I want to stress this doesn’t mean that this is for everyone. A lot of these conditions have only been discovered in the last few decades.
Many problems are going to be properly identified and labelled in the years to come. Really working on this and understanding all the different roles microbiota, the gut, mental health, physical health and the immune system play is so important for feeling the best version of you that you can be.
I hope that helped. There was a lot of information to take in, but the key thing is to look at your diet.
Strip out any ultra-processed foods and high sugar, concentrated sugar stuff.
Stay on top of your stress and try to take it easy where you can on overuse of anti-inflammatory drugs like ibuprofen and antibiotics where possible, where it’s safe to do so.
Be measured on alcohol.
If you can do those things, you will see profound changes. The evidence is overwhelming that if you eliminate the bad stuff, stay on top of your stress, don’t overdo it on the meds that are going to dramatically alter your microbiome, you’re going to feel so much better. I’m living proof of that.
Many people I’ve talked to have had life-changing effects from changing their diet, and I hope that can be the same for you as well.



0 Comments